Published: July 27, 2025
A pivotal study, published on July 24, 2025, in a leading neuroscience journal, has uncovered a critical consequence of the COVID-19 pandemic: accelerated neurological aging in individuals who never contracted SARS-CoV-2. Conducted by a distinguished team of neuroscientists at a premier United Kingdom research institution, this study leverages advanced neuroimaging to demonstrate that chronic stress and social isolation during pandemic lockdowns induced measurable brain changes comparable to premature aging. These findings highlight the urgent need for targeted public health strategies to address the enduring neurological and psychological impacts of the global health crisis.
Methodology and Principal Findings
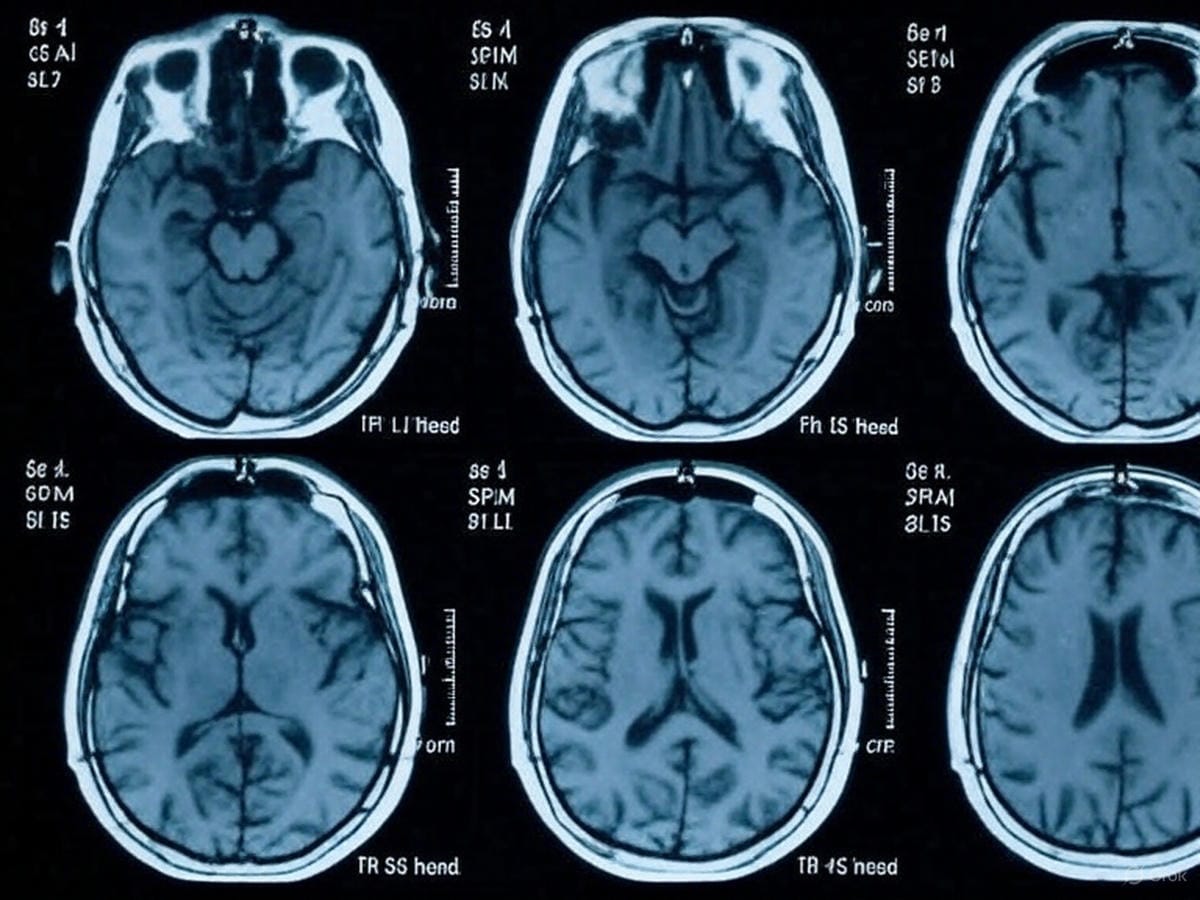
The investigation, led by neuroscientists at a top-tier UK academic institution, analyzed longitudinal neuroimaging data from a cohort of 1,127 participants, with brain scans collected before (2019), during, and after (2025) the COVID-19 pandemic. Employing high-resolution magnetic resonance imaging (MRI), the study focused exclusively on participants who consistently tested negative for SARS-CoV-2, isolating the effects of psychosocial stressors such as social isolation, economic instability, and disrupted daily routines.
The results revealed significant neurological alterations. Participants exhibited a statistically significant reduction in gray matter volume in the hippocampus and prefrontal cortex—regions essential for memory, emotional regulation, and executive function. These structural changes, typically associated with natural aging, indicate an accelerated neurological aging trajectory, equivalent to 1.5 to 3 years beyond chronological age. Cognitive assessments further confirmed declines in processing speed, working memory, and attentional capacity, particularly among those reporting heightened stress during the pandemic.
Mechanisms Driving Neurological Changes
The observed changes are attributed to the combined effects of chronic stress and social isolation. Prolonged stress elevates cortisol levels, a glucocorticoid that impairs neuronal integrity, disrupts synaptic plasticity, and accelerates neurodegeneration. Social isolation, a defining feature of lockdown measures, further exacerbates these effects by reducing cognitive stimulation and social engagement, both critical for maintaining neurological health.
Dr. Emily Carter, the study’s lead investigator, stated, “The brain relies on dynamic social and environmental interactions to sustain optimal function. The severe restrictions during the pandemic disrupted these essential inputs, resulting in measurable and persistent neurological consequences, even in those spared from viral infection.”
Demographic and Socioeconomic Variations
The study identified distinct variations in susceptibility across demographics. Younger adults (aged 18–35) showed more pronounced brain changes, likely due to disruptions in critical life stages such as education, career development, and social network formation. Women were disproportionately affected, potentially reflecting increased caregiving responsibilities and economic pressures. Individuals with pre-existing mental health conditions, such as anxiety or depression, exhibited the most significant gray matter reductions, underscoring the link between psychological and neurological vulnerabilities.
Socioeconomic factors amplified these effects. Participants from lower-income groups or those facing employment instability reported higher stress levels, correlating with greater neurological changes. These findings highlight the unequal distribution of the pandemic’s psychological burden and its potential to widen health disparities.
Public Health Implications

The findings carry profound implications for public health and clinical practice. Accelerated neurological aging, even by a few years, may increase the risk of cognitive decline, neurodegenerative disorders, and reduced quality of life in later years. The researchers advocate for comprehensive mental health interventions, including accessible telehealth psychotherapy, community-based resilience programs, and workplace policies to mitigate chronic stress.
The study also emphasizes the need to integrate neurological and psychological considerations into future public health crisis frameworks. Dr. Carter noted, “The neurological impact of prolonged psychosocial stress necessitates a paradigm shift in crisis response planning. Proactive mental health support is essential to protect long-term cognitive health.” Recommended measures include scalable virtual social engagement platforms, subsidized mental health services, and evidence-based campaigns promoting stress-reduction strategies, such as structured physical activity and mindfulness practices.
Strategic Recommendations for Stakeholders
The neurological legacy of the COVID-19 pandemic demands a coordinated response from policymakers, healthcare providers, and communities. Governments should prioritize sustained investment in mental health infrastructure, ensuring equitable access across socioeconomic groups. Healthcare systems must incorporate routine neurological screenings into post-pandemic care protocols to monitor and address cognitive changes proactively. Individuals are encouraged to foster social connections, engage in cognitively stimulating activities, and adopt evidence-based stress-management techniques to preserve neurological health.
This research serves as a compelling call to action to address the hidden neurological consequences of the pandemic. By prioritizing mental and neurological well-being through evidence-based interventions, society can mitigate the long-term impacts of this unprecedented crisis and build resilience for future challenges.
Source: Neuroscience Journal (July 24, 2025), United Kingdom Longitudinal Neuroimaging Study