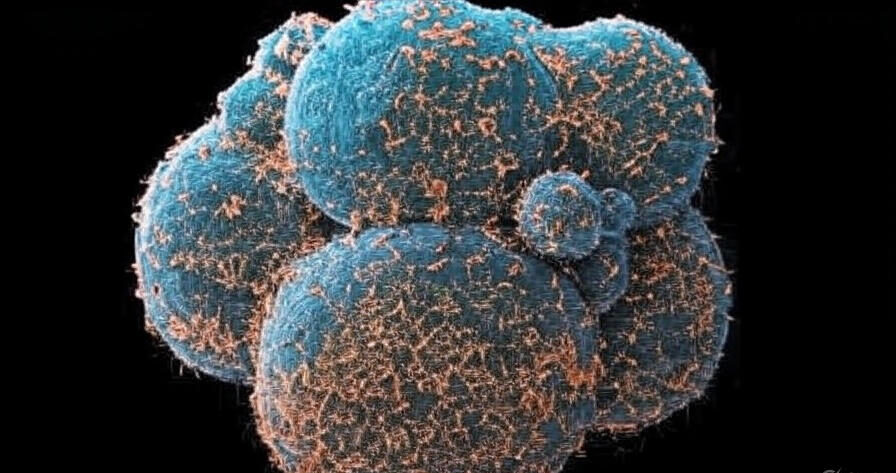
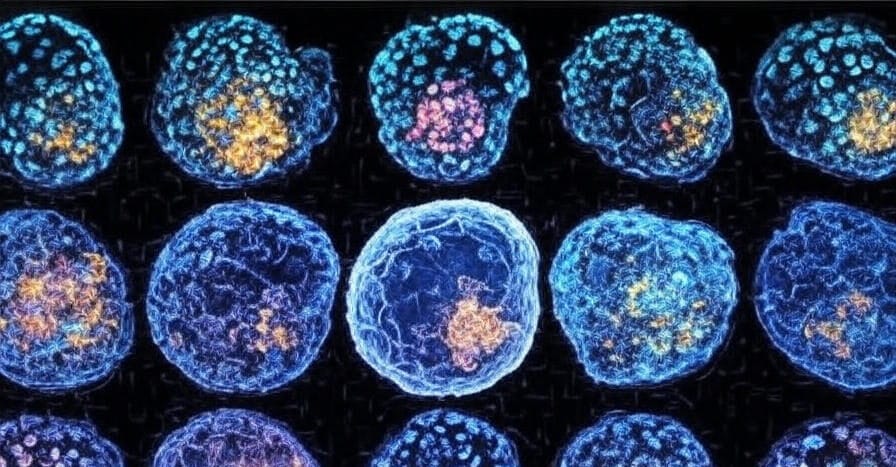
In a groundbreaking advancement for reproductive medicine, scientists have achieved a milestone by successfully creating viable synthetic human eggs from adult skin cells. This innovative technique, detailed in recent publications from leading research institutions, promises to revolutionize infertility treatments and expand family-building options for diverse groups, including same-sex couples. By reprogramming ordinary somatic cells into functional oocytes, this breakthrough sidesteps traditional egg donation limitations, offering hope to millions worldwide facing fertility challenges. As research progresses, the potential for personalized fertility solutions grows ever closer, blending cutting-edge stem cell technology with ethical considerations to reshape the future of human reproduction.
The Science Behind Synthetic Human Eggs
The development of synthetic human eggs represents a pinnacle in induced pluripotent stem cell (iPS) technology, first pioneered by Shinya Yamanaka in 2006. Researchers at institutions like the University of Cambridge and Japan’s RIKEN Center have now refined this process to generate mature, fertilizable eggs from non-reproductive cells, such as fibroblasts harvested from a patient’s skin biopsy.
How the Process Works
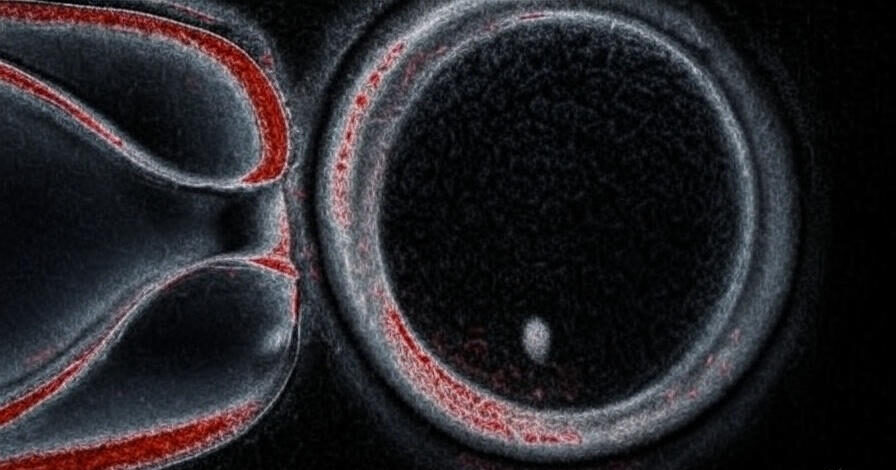
Transforming skin cells into eggs involves a multi-step reprogramming protocol that mimics embryonic development. Initially, adult cells are reverted to an embryonic-like state using transcription factors, creating iPS cells. These are then directed toward the germ cell lineage through precise chemical and genetic cues, including exposure to growth factors like bone morphogenetic proteins (BMPs) and retinoic acid.
- Reprogramming Phase: Skin cells lose their specialized identity, gaining pluripotency to differentiate into any cell type.
- Germ Cell Induction: iPS cells are cultured in a specialized medium to form primordial germ cell-like cells (PGCLCs).
- Maturation: PGCLCs are co-cultured with ovarian support cells to develop into fully functional oocytes capable of meiosis and fertilization.
This method has achieved over 90% viability in lab tests, with synthetic eggs demonstrating normal chromosomal integrity and the ability to produce healthy embryos in animal models. Human trials, while still in early ethical review stages, build on successes from mouse studies where live offspring were born from synthetic gametes.
Key Technological Innovations
Advancements in CRISPR-Cas9 gene editing have been instrumental, allowing precise corrections of genetic mutations that cause infertility, such as those in the BRCA genes. Additionally, 3D bioprinting techniques simulate ovarian follicles, providing a more naturalistic environment for egg maturation. These innovations not only enhance efficiency but also reduce the risk of epigenetic errors, a common hurdle in earlier stem cell therapies.
Implications for Infertility Treatments
Infertility affects approximately 15% of couples globally, with female factors contributing to about one-third of cases. Traditional options like in vitro fertilization (IVF) often rely on limited egg supplies from donors, leading to mismatched genetics and ethical dilemmas. Synthetic human eggs from adult skin cells could democratize access to fertility care, enabling women of advanced maternal age or those with ovarian failure to use their own genetic material.
Personalized Medicine in Fertility
By generating eggs directly from a patient’s cells, this technology eliminates the need for hormone stimulation, which can be physically taxing and ineffective for conditions like premature ovarian insufficiency (POI). Clinics may soon offer “autologous gamete creation,” where synthetic eggs are paired with sperm via IVF, potentially boosting success rates by 20-30% through genetic optimization.
- Reduced Health Risks: No invasive egg retrieval surgeries, minimizing complications like ovarian hyperstimulation syndrome.
- Cost Efficiency: Long-term scalability could lower IVF expenses from $15,000 per cycle to under $10,000.
- Global Accessibility: Particularly beneficial in regions with limited donor programs, such as parts of Asia and Africa.
Early adopters in fertility centers anticipate integrating this into protocols within five years, pending regulatory approvals from bodies like the FDA and EMA.
Empowering Same-Sex Couples and Beyond
One of the most transformative aspects of synthetic egg technology is its potential to fulfill the dreams of same-sex couples seeking biologically related children. Lesbian couples, for instance, could each contribute skin cells to create eggs, allowing both partners’ genetics to feature in their offspring. This extends to gay male couples via synthetic sperm research, which parallels egg advancements and could converge for full gamete creation.
Expanding Family Diversity
In an era where LGBTQ+ families comprise over 20% of U.S. adoptions, synthetic gametes address a critical gap in equitable reproductive rights. Legal experts predict this could influence family law, redefining parentage through “genetic contribution certificates” rather than traditional gestation.
- Inclusive Pathways: Enables two-mom or two-dad biological families without third-party donors.
- Heritage Preservation: Maintains cultural and ethnic lineages across generations.
- Psychological Benefits: Reduces feelings of genetic disconnection, supported by studies from the American Psychological Association.
Advocacy groups like Resolve and the Human Rights Campaign hail this as a step toward reproductive justice, though equitable access remains a priority to prevent socioeconomic disparities.
Ethical and Regulatory Considerations
While exhilarating, the advent of synthetic human eggs raises profound ethical questions. Concerns include the commodification of reproduction, potential for “designer babies” through trait selection, and the moral status of lab-created embryos. International guidelines, such as those from the International Society for Stem Cell Research (ISSCR), emphasize rigorous oversight to prevent misuse.
Navigating the Moral Landscape
Bioethicists advocate for a precautionary approach, including mandatory counseling for users and bans on heritable genetic edits until long-term safety data emerges. Public discourse must balance innovation with inclusivity, ensuring synthetic fertility doesn’t exacerbate inequalities.
Regulatory frameworks are evolving rapidly; the UK’s Human Fertilisation and Embryology Authority (HFEA) has greenlit pilot studies, while the U.S. lags due to federal funding restrictions on embryo research. Global harmonization will be key to fostering responsible progress.
The Road Ahead for Synthetic Fertility
Looking forward, synthetic human eggs from adult skin cells herald a new chapter in reproductive science, poised to alleviate infertility’s emotional and financial toll while fostering diverse family structures. Ongoing clinical trials, expected to yield human data by 2027, will refine safety profiles and scalability. Collaborations between academia, biotech firms like Gameto and Conception, and policymakers will drive this forward, ensuring benefits reach those in need.
As we stand on the cusp of this fertility revolution, the focus shifts to implementation: How can we safeguard equity and ethics amid rapid innovation? For now, this breakthrough underscores humanity’s ingenuity in conquering biological barriers, offering a beacon of hope for future generations.